Sharing The Surgical Schedule
By: Sherwyn D’Souza | Project Partner: Alice Ng
Project Supervisors: Dr Michael O’Sullivan Jr. and Dr Tava Olsen
The Surgical Supply Chain
Methodology
Demand
Lead Time
EOQ
Safety Stock
This is an additional quantity of an item held in inventory to reduce the risk that the item will be out of stock. The safety stock acts as a buffer in-case demand is larger than expected. ggggggggggggggggg
ROP
Reorder point (ROP). As the name implies this is the inventory level at which the central warehouse will send out an order of size EOQ to the manufactures. We created a tool to calculate this for items that come in loan sets.
The Surgical Inventory Process
The videos below demonstrate the logic in the EOQ model for hip implants. The video on the left demonstrates the process hip implants go through to get to the patient. The video on the right demonstrates how the inventory level of hip implants change in the central warehouse over time. We then build a numerical simulation to model these processes.
Results
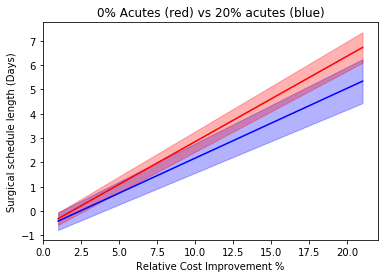
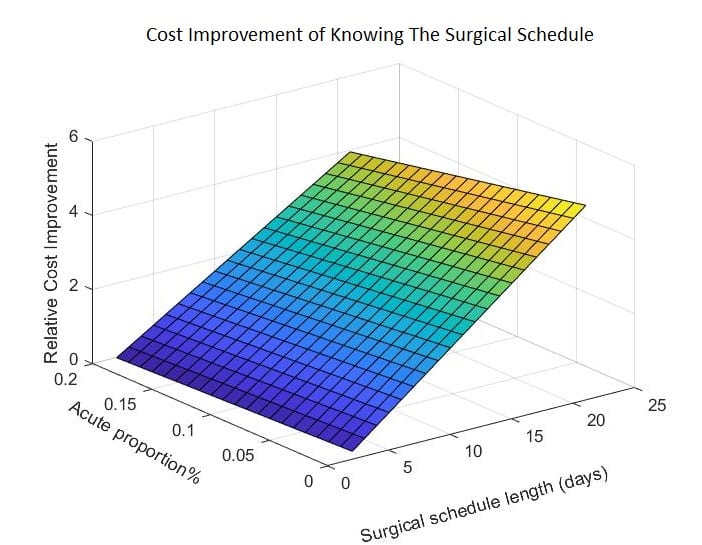
The main experiment run was simulating the relative cost of not having a surgical schedule against the length of the surgical schedule, i.e. how many days of lead time demand can the surgical schedule provide. In this experiment, we considered ten different surgical schedule lengths, ranging from two to twenty days, and four different proportions of acute surgery (0%, 5% 10% and 20%). The simulation was repeated ten times for each surgical schedule length and acute surgery proportion, to get a 95% confidence interval. We found that the central warehouse can expect to save around 3.7% of its inventory management costs or $7000 per year if it were to use the fourteen-day surgical schedule from a typical hospital.
Conclusion
The aim of this project was a proof of concept to determine whether knowledge of the surgical schedule will be valuable to the central warehouse. We developed a tool that uses surgical schedule information to calculate the reorder point of surgical equipment that come in loan sets. We developed a simulation to quantify the savings the central warehouse can make if they use the surgical schedule to make their purchase decisions. We found that the central warehouse can expect to save $7000 (3.7%) of inventory management costs of hip replacement surgeries. In the future, this model can be expanded to model all loan sets used in the hospital, to get the total cost that the central warehouse can save on all loan sets.

